Clinical Programs and Medication Adherence
Buckeye Health Plan offers tailored clinical programs that are customized to drive medication adherence and reduce medication errors. These programs are designed to improve health outcomes by supporting members in managing chronic conditions and ensuring they receive the right medications at the right time to get and stay healthy.
Medication Therapy Management (MTM): Our MTM programs support members in understanding and managing their medications, helping to optimize their health regimens and improve therapeutic outcomes.
EQUIPP
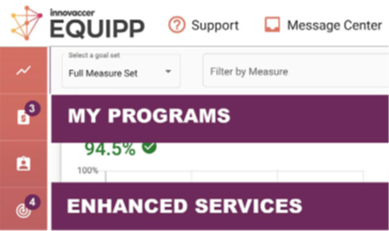
Buckeye Health Plan has partnered with Pharmacy Quality Solutions (PQS) to offer a Longitudinal Adherence Monitoring Program (LAMP) through the EQUIPP platform. EQUIPP is a data-driven performance platform that allows pharmacies to measure, track, and improve medication-related quality measures and other patient care initiatives. See below for more details on this unique tool.
Increase the revenue for your pharmacy by implementing the 2025 Buckeye Health Plan Pharmacy Network Program and Enhanced Services
into your pharmacy workflow.
The pharmacy role is expanding dramatically, moving beyond medication dispensing to active participation in clinical care. As essential members of the healthcare team, pharmacists can generate new revenue streams through compensation from Buckeye Health Plan for medication adherence, bonuses for therapeutic outcomes, and income from intervention led services all by accessing the EQUIPP platform.
In the first quarter of 2025, Buckeye Health Plan launched a program that offers pharmacies incentives to close care gaps in EQUIPP and is accessible via the “My Programs” tab on EQUIPP. This program evaluates performance across key medication-related quality measures along with formulary adherence and provides reimbursement to pharmacies who meet established population-level performance goals.
Closing Gaps in Care, including the Longitudinal Adherence Monitoring Program (LAMP) and HEDIS® (CBP) programs launched April 2025. Utilize the target (bull’s eye) icon in EQUIPP to access Enhanced Services to view patients for both LAMP and HEDIS opportunities to close gaps in care and earn revenue.
Log in today! Equipp
RxEffect
Buckeye Health Plan partnered with RxAnte to offer an innovative quality platform called RxEffect, which enables providers to improve medication adherence for both Medicare and Ambetter patients. This platform is free to provider groups and offers targeted patient lists, daily claim updates, and strong workflow support for your practice to support medication adherence. Active use of the RxEffect tool has improved adherence and quality measure outcomes. See below for more details on this unique tool.
1st subsection under RxEffect Header titled “RxEffect Incentive Payment for Stars Adherence Measures (Medicare)”
- Please change the title of this section to just “RxEffect Incentive Payment for STARs Adherence Measures”
- Please use the attached WORD document to copy the blurb under this header so all of my updates will be there
3rd subsection under RxEffect Header titled “RxEffect Medication Adherence Program”
- Please use the attached WORD document to copy the blurb under this header so all of my updates will be there
Please note: The communications to introduce this program have used the incorrect product name. This program is for Medicare Only at this time.
As part of efforts to improve medication adherence, additional financial incentives (Incentive Payment Program) are offered to our providers who use RxEffect® to identify and take action in the following STAR ratings medication therapy areas:
- Diabetes
- Blood Pressure
- Cholesterol
In addition, incentives are offered for identifying and taking action on the following other prescribing opportunities:
- Statin Rx for Diabetes
- Statin Rx for CVD
- Med Overlap – ACH
- Med Overlap – CNS
- Med Overlap – opioids and benzos
Please note: the RxEffect tool can be utilized for both the Medicare and Marketplace (Ambetter) lines of business.
This Program Description is the governing document regarding the Bonus amounts that a provider is eligible to earn under this Incentive Program.
Definitions:
- Adherence is defined by the Proportion of Days Covered, or PDC. PDC is “the proportion of days in the measurement period ‘covered’ by prescription claims for the same medication or another in its therapeutic category.” It is the total number of days that a member has medications on hand divided by the number of days in the measurement period. Members are defined as adherent if they have a PDC ≥ 80%.
- In order to track treated days consistently, it is important that Eligible Members fill their medication at a pharmacy or through home delivery using their health insurance card.
- Missed Days means the number of days an Eligible Member does not have prescription medication on hand to treat their chronic disease because the Eligible Member did not refill his/her medication on time. The incentive program uses Missed Days to measure adherence.
- Bonus means the additional reimbursement beyond the contract rates in the participation agreement a provider may receive. This is a separate bonus program that supplements, but does not replace, any other Plan programs or risk-based contracts in which providers may be enrolled.
- Eligible Member means a Plan member who meets the age, sex, and/or disease-specific criteria, and the enrollment and other technical criteria, set forth in the most recent Centers for Medicare & Medicaid Services (CMS) Medicare Part C & D Star Rating Technical Notes document.
Medication Adherence Measures
Diabetes | Blood Pressure | Cholesterol |
|
|
|
- Qualifying Member Therapy means the three Medication Adherence Measures published in the most recent CMS Medicare Part C & D Star Rating Technical Notes document, namely (1) Diabetes Medication; (2) Hypertension (RAS Antagonists); and/or (3) Cholesterol (Statins).
- Star Ratings mean the CMS Five-Star Quality Rating System for Medicare Advantage plans.
Incentive Payment Program Criteria:
This Incentive Payment Program offers additional incentive dollars per Qualifying Member Therapy for a bonus period. This program occurs between August of the current year or date of program launch, through December 31st of the current year. The Bonus is based on Eligible Members getting their last medication fill for end of year adherence, and is broken into two categories:
- “Extended Day Conversion” – The Bonus icon will appear for member therapies converted from a 30-day fill to a 90+ day fill that makes the Eligible Member adherent for that therapy.
- “Last Fill” – The Bonus icon will appear for Eligible Member therapies that need one fill to meet the Eligible Member’s adherence goals for that therapy.
Bonus eligibility is dynamic and will be updated weekly. Please note: While a Qualifying Member Therapy may be eligible for each of the Bonus types through year-end, only one Bonus will be active at a time and therefore only one Bonus will be paid per therapy.
Incentive Payment Program Eligibility
To receive your Bonus, you must take the following steps:
- Visit RxEffect website External Link to review the Qualifying Member Therapies eligible to receive a Bonus. The patient list must be viewed while the therapy is eligible to receive a payment.
- Help ensure the Eligible Member meets adherence criteria by filling a pharmacy claim through their prescription benefit (without a claim reversal) for that therapy area while eligible for the Bonus (displaying the Bonus icon).
How to Identify Bonus Opportunities in RxEffect
The RxEffect features in the patient portal will help you improve your adherence population and start earning incentives.
- Priority List: The Priority List ranks patients based on their likelihood of becoming adherent and responding to an intervention, bonus eligible opportunities and patients will exist in this list among other prioritized patients.
- Bonus Icon: Select high-priority patients who are eligible for an additional bonus will be represented by a dollar sign on the therapy tile. If a patient has a bonus icon on each adherence therapy, you can earn up to three Bonuses for that Eligible Member.
- Bonus List: Click on this list to show all Bonus Eligible Patients for the current calendar year.
- Missed Days: Keep patients under their targeted number of missed days on each therapy tile and they will be adherent for the calendar year.
Incentive Payment Program Payout
Incentive Payment Program payout will be included as a separate line item for the following calendar year.
View your Progress
Located in the Reports tab on RxEffect, this dashboard will show your completed Incentive Payment Program earnings and remaining potential. View these opportunities overall for a practice or filter to an individual provider. Reports will be updated daily as eligibility is updated.
Access to RxEffect
If you do not currently have access to RxEffectExternal Link, please contact help@RxEffect.com. If you have questions about the bonus program, contact your Health Plan representative or call Provider Services at 866-593-1831 (TTY 1-877-247-6272) Monday–Friday 8 a.m. to 9 p.m.
Disclaimers:
- The Plan reserves the right to not pay any Bonus to a provider if the provider has received or retained an overpayment (any money to which the provider is not entitled), as determined by the Plan. In the event the Plan determines a provider has an overpayment, the Plan may offset the overpayment by any Bonus payment that may have otherwise been paid to the provider.
- The Plan will determine if the requirements of the Incentive Payment Program are satisfied, and Bonuses paid under the Incentive Payment Program will be paid solely at the Plan’s discretion. The Incentive Payment Program does not provide any right(s) to appeal a decision made in connection with the Incentive Payment Program.
- Plan shall make no specific payment, directly or indirectly under a physician incentive plan, to a provider as an inducement to reduce or limit medically necessary services to an enrollee. This Incentive Payment Program does not contain provisions that provide incentives, monetary or otherwise, for withholding medically necessary care.
- The Plan’s Incentive Payment Program is discretionary and subject to modification due to changes in government health care program requirements, or otherwise.
- RxEffect® is a registered trademark of RxAnte, LLC.
We all know the importance of medication adherence and how that alone can have more of an impact on health outcomes than the specific treatment itself. It is critical that we focus on helping patients understand the importance of taking their medications, as prescribed, to maximize the potential benefits for their corresponding chronic disease to improve their overall quality of life.
Starting the conversation now on taking medications, as prescribed, will set up your patients for success throughout the year and help you achieve patient care goals. Some key points to remember regarding medication adherence:
- According to the CDC and WHO, about 50% of medications for chronic diseases are not taken as prescribed.
- Lack of adherence causes higher rates of hospital admissions, suboptimal health outcomes, increased morbidity and mortality, and increased healthcare costs.
Looking at these key points, what can you do to help? The most important thing you can do is to listen to patients and truly understand the barriers they are having. This will help develop more impactful medication adherence initiatives and improve overall patient outcomes. From there, making changes like converting medications for chronic diseases to extended day supplies, up to a 100 day supply, will result in a significant boost in medication adherence across the board.
Utilizing tools like RxEffect can help you prioritize your most critical patients and streamline your conversations to get to the root cause of medication non-adherence. This will enable you to address the medication adherence barrier and close several gaps in care in one sitting. If you haven’t yet, check into RxEffect to see how it can help you achieve your goals. As always, our team is here to help you in any way we can!
Tips
Listening
Ask questions. You can’t help close barriers if you don’t know what they are. Are they taking all their medications? If not, why?
- How often do you miss one?
- Financial concerns
- Forgetfulness
- Side effects
- Don’t feel they need them
Understanding
Address any barriers:
- Educate/explain side effects
- Provide written instructions
- Brainstorm solutions to scheduling issues
- Share resources for financial assistance
- Utilize health literacy tools to help you, help them.
- Reduce the complexity of the drug regimen
Are you aware that out of every 10 of your patients, three may not be taking their medications as prescribed and one of those may require hospitalization as a result?
To assist you, we are excited to offer you our RxEffect Medication Adherence Program for your Medicare Advantage patients. The program features the ability to promote extended day supply Rx use, statin use for patients with diabetes and several other features.
A 2019 study shows that providers using RxEffect have a 3.5 times greater adherence rate in their patient population than those providers that do not use the program.
With RxEffect you are able to:
- Easily track patients at risk of becoming non-adherent
- Earn additional dollars in incentives per member
- Improve Medicare STARs scores
You can access the RxEffect web-based portalExternal Link at this link.
Contact your Buckeye Provider Relations Representative for more information!
The RxEffect platform is a valuable tool that assists you in identifying patients that are non-adherent to their diabetes, hypertension, and cholesterol medications, as well as assisting with identifying varying gaps in care for this specific Medicare population. We've had several provider groups utilize this tool frequently, resulting in improved medication adherence leading to better Medicare STAR ratings and increased success in varying HEDIS measures, as well as improved quality of life for our members! Below are a few examples from provider groups on how they utilize the platform and best practices that have helped them fit these opportunities into workflow.
Ohio PCPs & Specialists
RxEffect User Base:
Pharmacy Resident
BEST PRACTICES
- Enjoys the RxEffect platform and its ability to sort and prioritize non-adherent patients for outreach
- Chart review is completed, and documented therapy is discussed with authorizing provider prior to patient outreach
- Once patients are contacted, they are educated on medication adherence and the importance of taking medications to control chronic disease and improve quality of life
- Local pharmacies are contacted for refills on behalf of the patient if needed
- Large focus within provider group on diabetes, hypertension, and cholesterol medication adherence; thus, RxEffect fits right into workflow
- Another focus for the provider group that RxEffect has assisted with is gaps in care regarding statin use in patients with diabetes and ACE-I/ARB use in patients with micro/macroalbuminuria
Ohio PCPs
RxEffect User Base:
Care Manager
SUCCESS STORY
“A patient had been discharged from a SNF a few weeks prior to my initial outreach. The outreach uncovered the patient was taking leftover medications from before his hospital, then SNF stay, and was running out. The patient shared he was unsure of how to handle this and shared that he did not receive any prescriptions from the SNF upon discharge.
I reviewed the patient’s medications in EPIC and found that all the medications the patient was discussing were listed in his medication review. However, when each medication was opened to do additional research, I discovered none of the patient’s prescriptions were active. From there, I requested paper script orders of each medication that had been hand delivered to the SNF by the ambulance company when delivering the patient. In addition, I contacted our internal pharmacy to verify the patient had no active scripts. Once everything was sorted out, I sent a message to the patient’s PCP regarding the situation and notified them that he needed all his medications reordered. A few days later the patient visited his PCP and was able to receive new prescriptions.”
South Carolina FQHCS
RxEffect User Base: Nurse
BEST PRACTICES
- I absolutely LOVE RxEffect! I check RxEffect every single day, except on weekends, to see where my patients stand with medication adherence and ensure that all my patients have medications on hand.
- I do get assistance from my two pharmacist peers with this platform and between all of us we can even pick up the phone and call our community partners at retail pharmacies to see if they can refill medications for our identified patients if needed or even add our patients to adherence programs (such as automatic refills or one trip refills).
- I do get assistance from my two pharmacist peers with this platform and between all of us we can even pick up the phone and call our community partners at retail pharmacies to see if they can refill medications for our identified patients if needed or even add our patients to adherence programs (such as automatic refills or one trip refills).
- I try to break down barriers in medicine by educating people on the fact that adherence oral diabetes medications, blood pressure medications, and statins are monitored by Medicare to help them improve their quality of life and ensure that healthcare professionals are educating and supporting patients as needed.
- I explain that because of this outreach, we can help patients understand their medications and reduce the risk of strokes, heart attacks, and diabetic crisis.
- I also explain that eating healthy, getting exercise, drinking water, and keeping appointments with their primary care physician goes hand in hand with medication adherence to improve quality of life.
- The number one thing I do when speaking to patients is I break down medications and medication adherence into simple terms that anyone can understand.
- Patients with diabetes seem to understand what their oral diabetes medications are doing for them; they know that it lowers their blood sugar, and they know that they do not feel good when their blood sugar is too high or too low.For blood pressure medications, I try to explain how they benefit our patients through an analogy.
- Think of your body as a toy car on a toy car track. The blood is the car, and the blood vessels are the car tracks. The “garage” that the car would fill fuel at on the toy track would be the heart. As the car moves along the car track, you can visualize how blood moves through the vessels. When you have a car (blood) charged up by the garage (heart), the car (blood) will leave the garage (heart) faster paced and return to the garage slower paced. This analogy also represents blood pressure, where the top number would be the “speed” leaving the heart, and the bottom number would be the “speed” returning to the heart. If the car (blood) comes back to the garage (heart) too fast paced, the car could wreck the garage door. Thinking of that happening in your body, the more your blood returns to the heart supercharged and beating on the heart valves, the more damage you can cause to the heart valves and the heart muscle itself.
- For statins, I try to explain how they benefit our patients through a slightly different analogy.
- Think of your blood vessels as plumbing in a house. The blood vessels are like drains of the house and when the blood vessels get clogged, similarly to a drain, they cannot filter fluids as easily and need to be unclogged. So, just like drains fill with junk and clog them, blood vessels can fill with cholesterol and clog them. A statin would be what you would use to “unclog” your blood vessels, similarly to how products like Draino would unclog a drain in your home.
- Getting patients adherent to cholesterol medications was the biggest challenge when initially starting RxEffect but we have improved adherence so much that our opportunity list has dropped from thousands of members to less than one hundred members.
- It is an amazing thing to see the great success we have had, with patients becoming more compliant, getting the healthcare they need, and truly understanding why they are taking medications.
- Patients with diabetes seem to understand what their oral diabetes medications are doing for them; they know that it lowers their blood sugar, and they know that they do not feel good when their blood sugar is too high or too low.For blood pressure medications, I try to explain how they benefit our patients through an analogy.

